“What I do next will be of direct benefit to the people I knew at the start of my journey, in the hospitals of Sub-Saharan Africa, where the diseases I now research in the laboratories of Cambridge are so prevalent.”
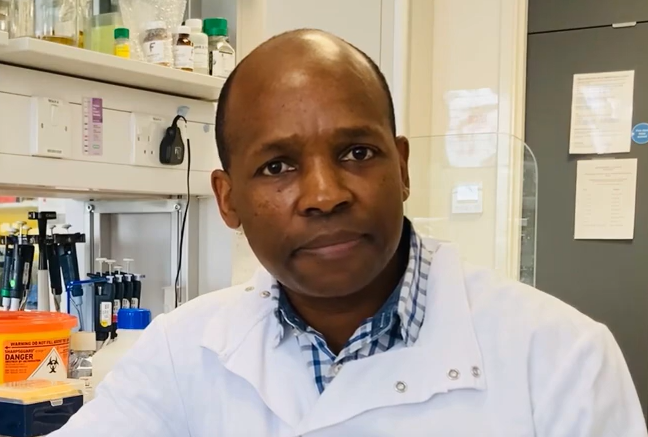
Dr Nyaradzai (Nyarie) Sithole, Hughes Hall Research By-Fellow, identifies the turning points, coincidences and kindness that helped chart his advance across the globe, tackling different pathogens, and building up clinical and research expertise in order to effect change in the region he came from.
“I trained as a medic in my home country of Zimbabwe and served a few years as a junior hospital doctor – this is where I felt my future lay – in clinics, by people’s bedsides. I supplemented this training with a UK Master’s degree in Tropical Medicine and Infectious Diseases which was a special interest of mine. During this time, I had my first taster of lab-based research which proved to be a turning point.”
“I thought being a clinician was the pinnacle of things for me but there was also a deeper feeling that this wasn’t my end-point. I begun to seek a role that combined primary research as well as the rewarding work with patients, but I hadn’t come across lab-led research before coming to the UK.”
During his Master’s degree, Nyarie looked at the effect of vaccination on Rotavirus using data gathered from a largescale vaccination programme in Brazil to understand how the vaccine impacted the epidemiology and landscape of Rotavirus in Brazil. Inspired, he went on to accept a job at Addenbrooke’s as a Registrar in Infectious Disease but it was a short-term post so a risky choice over a longer term, more secure role, he had been offered elsewhere. Having taken up the Registrar role, the wards of Addenbrooke’s presented new opportunities, and discussions with senior colleagues proved inspiring.

“Something just said to me, Cambridge is where you need to go. This is where your research career is. I took the risk and I haven’t regretted it.”
“I was asked whether I’d consider pursuing a research role alongside my clinical work. Opportunity is a funny thing – sometimes it just presents itself to you during a spontaneous chat with a colleague in a lift when you haven’t slept for 18 hours!”
“It is a blessing to have inspiring colleagues who can see your potential when you’re too busy to notice it yourself. Professor Andrew Lever helped me take advantage of new opportunities in research which allowed me to gather the preliminary data which led in turn to my successful application for PhD funding.”
With Prof Lever’s support, Nyarie secured Wellcome Trust funding for new work on HIV replication in human cells. Nyarie’s PhD research elucidated essential domains of DEAD box helicases, DDX5 and DDX17, critical for their roles in HIV replication. It was a key step in bringing together clinical experiences in Zimbabwe treating people with HIV, with his early stage research career in the UK examining the action of the virus at cellular level. It was also the start of building bridges with clinicians in lower resource settings – to make a difference through new research to those places he used to work on the frontline.
As part of his post-doctoral fellowship, he was appointed to a clinical lectureship position with NIHR which again combined research and clinical work in infectious diseases. It was a perfect next step, and chance to further his HIV work, but one which involved another difficult choice as he’d also been offered a more secure full-time role as a NHS consultant. He made his second risky choice. But then came the pandemic and great change.
“The pandemic was serendipitous in a way. Whilst it derailed my HIV research momentum, I still managed to complete my training to become a consultant in infectious disease, and I set out on a new path, with a new virus.”
Nyarie treated some of the earliest COVID patients in the UK – at Addenbrooke’s – and went on to help establish the national response to long-COVID. In May 2020, he set up the first long-COVID clinic in Cambridge to assess patients referred by their GPs, who suspected they had had COVID-19 and were experiencing ongoing symptoms. Amongst other priorities, the clinic provided clinical service/management for patients with long-COVID and acted as a research hub for scientists and clinicians to research into the pathophysiology behind condition. This enabled him to use his infectious disease lab expertise in collaboration with other researchers, and his clinical work, which led in turn to a ground-breaking national role in long-COVID research.
“This combined my skills and expertise in vaccination, virus replication and wider epidemiology with my ongoing passion for working clinically with patients. The clinics were – and still are – transformational. Unknown to us, we were world-leaders; proactively pushing boundaries in this new urgent area of research. And, it was enormously valuable to develop my own immunology research expertise.”
“We knew from the wider infectious disease field that, for other diseases, patients rarely have symptoms that continue like this long after the initial infection. Perhaps general malaise but we’d never seen anything like long-COVID in terms of both the severity and the variety of symptoms. Every system in the body can be involved in a great wave of symptoms that comes and goes, and can significantly affect long-term health. This was new. So we set about understanding whether it is due to the immune response or some other dysregulated function. What we’ve learned about the body’s immune response to COVID, and therefore how to treat long-COVID, has had significant implications elsewhere in pathogen research and global epidemiology.”
Sharing findings, and research interests, with a former colleague in the US via Zoom during the pandemic, has led to another of those serendipitous opportunities, and Nyarie has found a way to unite new techniques in immunology research with previous expertise in order to address another disease: Tuberculosis.
“Like HIV, Tuberculosis is a disease which has effected Zimbabwe and much of Sub-Saharan Africa. I am taking the skills, techniques and expertise I gain from my work in the UK to address these big global health challenges. When I look back the journey makes sense; the bedside attendance in Zimbabwe to the labs of Cambridge and soon California.”
Nyarie has recently been awarded a prestigious five year Wellcome Trust Early Career Development award to investigate the mechanisms of antibody mediated protection against Mycobacterium tuberculosis. He will spend two years at the University of California, San Francisco, to learn and develop expertise that he will then bring back to the UK. His work will advance the knowledge of how the body’s immune system protects and helps to fight against Tuberculosis and he hopes the findings will ultimately help to design effective vaccines against TB.
“Ultimately, I plan to establish my own research group back in Cambridge, building on all I have learnt and the networks I have created up to that point; combining lab techniques, data analyses, immunological knowledge, clinical experience and epidemiological expertise, and bringing everything I have learnt from Africa, the US and the UK together.”
“Most rewarding of all, there is a cyclical aspect to the progression of this work – and of my own personal journey. The passion that lit for medical science as a new student back home has carried me through clinical and research settings, and through extremely demanding work schedules, many miles apart. “What I do next will be of direct benefit to the people I knew at the start of my journey, in the hospitals of Sub-Saharan Africa, where the diseases I now research in the laboratories of Cambridge are so prevalent.”
His work will focus on new aspects of the study of TB to determine the role of antibodies in protecting against the disease.
“Historically we have looked at the other arm of the immune response – the T-cells – but I will examine the roles that antibodies play and how they protect against tuberculosis. This will involve what I leant in the long-COVID clinic and allow me to harness my immunological knowledge for a new pathogen; and will take me down memory lane in terms of understanding a disease I tried to treat as a medical student in hospital in Zimbabwe.”
The University of California. San Francisco. is a world leader in the field of TB research so this is an important new step but Nyarie will remain involved with the long-COVID clinical research – that work is still unravelling new data and influencing practice and global research strategy and he has unfinished objectives: to help come up with novel therapeutics against long-COVID.
“I can’t say I planned this journey. Looking back it appears coherent but actually there were so many points of indecision, chance and putting myself ‘out there’ that led to now. Don’t be scared to approach senior people – you can find clarity and inspiration in other people’s words, and don’t let setbacks get in the way – every ‘failure’ leads to a new place and helps create the story of how you reached today.”
“The Hughes Hall postdoc community is a diverse and inspiring one – full of so many people doing different and brilliant things. I just wish I had more time to meet up with my peers but my new son is currently taking up all my free time. Let’s see what he makes of California!”
Further information
For more on Nyarie’s long-COVID work: https://www.hughes.cam.ac.uk/about/news/covid-19-the-long-and-short-of-it/.
Recent publications from Dr Sithole on long COVID:
Nyarie is a Clinical Lecturer in Infectious Diseases at Addenbrooke’s Hospital. After completing his MBChB degree in Zimbabwe, he was awarded the British Chevening Scholarship to undertake the MSc in Infectious Diseases and Tropical Medicine at LSTM (Liverpool), where he was awarded the Glen Williams Prize for the best student. Driven by his passion and vast experience in managing HIV patients, he was awarded the 2011 Evelyn Trust Research Fellowship and built on that to be awarded a Wellcome Trust Clinical Research Fellowship. He attained his PhD from the University of Cambridge. During his PhD he elucidated essential domains of DEAD box helicases, DDX5 and DDX17 critical for their roles in HIV replication.
He is passionate about building bridges with academic clinicians in low resource settings and is actively involved in setting up collaborations with researchers in Africa and Mexico.
He is a Fellow of the Royal College of Physicians (London) and previously served as a question bank contributor for their Medical Masterclass website.
22.03.23





